Checking Eligibility for Medicaid was the Norm for 55 Years.
The Unwinding Begins to Once Again Limit the MA Rolls to Those Eligible.
Medicaid programs across the nation finally return to business as usual – providing taxpayer-funded benefits only to those who are eligible – resuming normal operations where recipients are asked to show they still qualify for the program in order to renew and retain coverage.
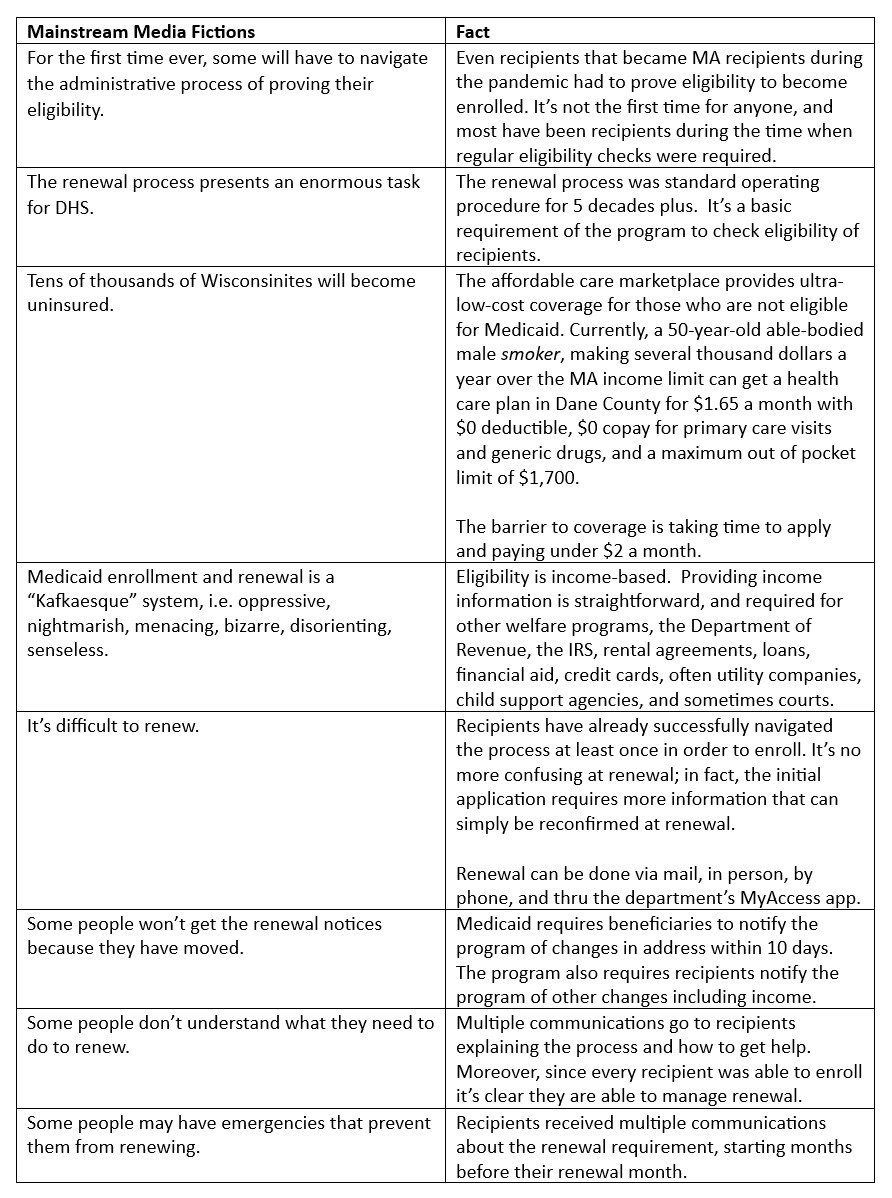
As we predicted, the mainstream media is pumping out stories about cruel eligibility checks leaving people without health coverage.
While an unbiased, unemotional summary might say ‘Millions of people who do not qualify for government benefits reserved for low-income people living in poverty are removed from Medicaid rolls, as program integrity is restored to the largest, most costly means-tested transfer program in the U.S.,’ PBS screamed “Millions may be kicked off Medicaid.’
Background
Three years ago, during (and well past) the pandemic, Medicaid programs across the nation stopped asking for income information from enrollees. The Trump Administration told states the federal government would pay a higher federal match rate as long as states did not continue asking beneficiaries to prove they were eligible during the health emergency. The feds called this “continuous coverage” and the Biden administration continued the health emergency and this ‘deal’ until April 1, 2023, when states were allowed to start asking recipients to show proof of income and stop providing benefits for those no longer eligible without losing the extra federal cash.
To be clear, states could have rejected the additional federal match cash and continued to check eligibility if they so desired. None chose to keep the integrity of the program by limiting it to those who actually qualified for the benefits. Instead, they all chose the federal cash.
It’s also worth noting that the federal government did not prohibit states from checking eligibility to get the enhanced match monies, only from disenrolling beneficiaries. States could, and should have been asking recipients to provide income information as usual and informing them of whether or not their income level would make them ineligible when the emergency ended. This would also have allowed states to have a better estimate of how many recipients were likely no longer to receive the benefits and kept recipients in the habit of providing renewal information. But none of the states chose to do that either.
The higher federal match dollars will phase out over 2023, and Medicaid rolls will still be bulked up with many ineligible recipients until mid-2024. States will bear higher costs as ineligible recipients continue to receive benefits and the federal money is pulled back.
Medicaid and Income
Medicaid is for people in poverty. Income is THE eligibility crux for Medicaid. You do not qualify for benefits if you don’t meet the income eligibility requirements. Even citizenship is not mandatory to receive Medicaid benefits (though there are few non-citizens receiving benefits), but low income is.
Income is the primary criteria because the nearly 60-year-old program was started to provide health care coverage for those in poverty with an emphasis on mothers, dependent children, the disabled and elderly. (Eligibility for Medicare, which provides health coverage for the disabled and elderly, is not based on income, though premiums may be imposed (and/or higher) for individuals with income over $97,000/year.)
Low income has been the baseline requirement for Medicaid eligibility for all of the program’s 58 years, but for the past 3 years, beneficiaries were not asked to prove they were financially eligible to continue to receive the generous, taxpayer-funded health care coverage.
And on those income limits: the income threshold for a childless, able-bodied, working age adult is $14,580 per year, a couple with three children can make over $105,000 per year and the children will be eligible for Medicaid. In historic low unemployment rates, Wisconsin has 300,000 able-bodied, childless adults taking Medicaid compared to 385,000 children.
Medicaid Enrollment Explosion
As one might expect, when eligibility requirements were removed for continuing Medicaid enrollment, the rolls exploded. In Wisconsin, we went from roughly 1.2 million recipients in December 2019 to 1.6 million in April 2023.
States have been planning for more than a year how to manage the “unwinding” of Medicaid continuous coverage by once again checking eligibility of beneficiaries, something that was done for over a half century with little Sturm and Drang. Most states, including Wisconsin, settled on a year-long unwinding process where beneficiaries would not all be asked to verify their income all at once. The vast majority of states chose a year-long unwinding period.
Among the reasons for the long timeline were the difficulty to manage the inevitable problems that would arise when people who couldn’t be bothered to renew lost their benefits and then found they could be bothered to complain. In other words, Medicaid, providers and stakeholders all knew this was coming, and spreading it out over 12 months makes it more manageable.
(A cynic might also posit that it also extends the news stories of how millions of people are being left without health coverage and dying because Republicans refuse to institute Medicare-for-All well into the campaign cycle.)
Kafkaesque?
In another time, taking benefits that you don’t qualify for would be considered fraud, but for the past three years and until the unwinding is complete, it’s been OK with the government.
We are only weeks into what we can expect to be at least a year of stories about the onerous problems caused by having Medicaid recipients provide basic information (information they managed to provide to enroll) to confirm they remain eligible for the taxpayer-funded health care benefits. The left is using this opportunity created by stories of lost coverage to push public opinion toward their goal of universal, government-run health care.
Here are a few examples of language the mainstream media is using to hyper-hype the left’s narrative of how problematic it is to ask that in return for free, generous healthcare coverage, recipients prove they remain eligible.
Difficult and Confusing?
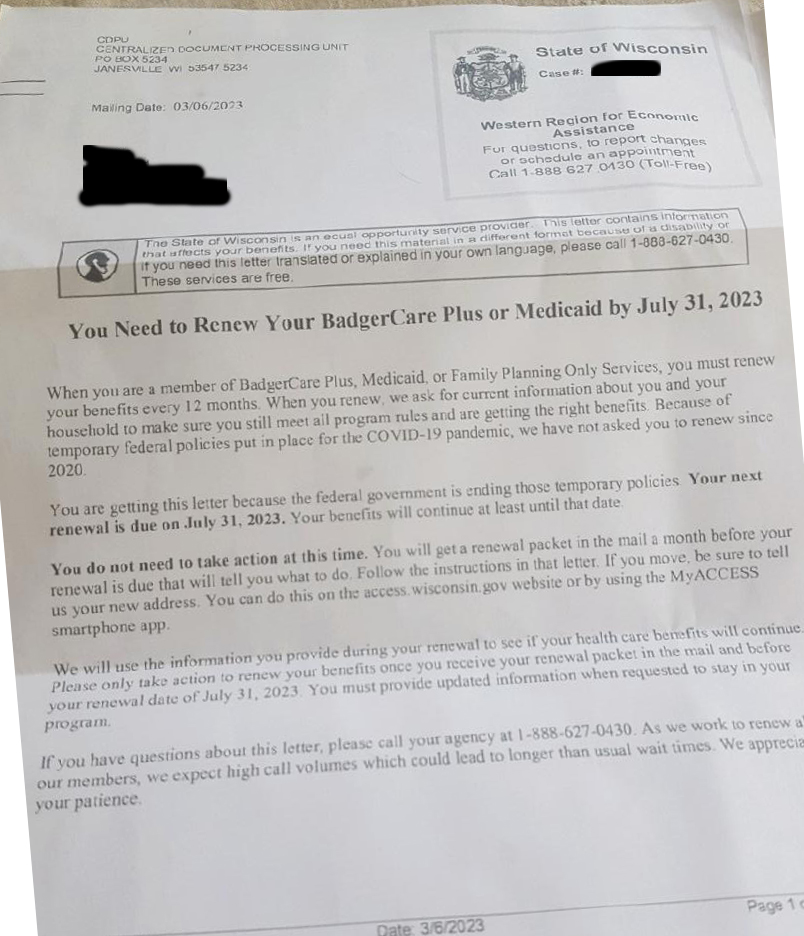
For those who are required to renew by July 31, a letter was sent in early March explaining that they would be required to renew, that they would be receive a renewal packet at a later date and providing contact information for the department. As an example:
- The letter pictured below was sent March 6th, 147 days ahead of a renewal due July 31st. It is simple and clear, hardly Kafkaesque.
- A renewal packet arrived in mid-June, which was due by July 31 containing the previous information the department had on file and asking the recipient to make changes (if applicable) and return the information with any required documents (pay stubs, etc.).
- Renewal can be done by mail, in person, on the phone, or in the state Medicaid app.
It’s not a heavy lift. Recipients have renewed for 55 years, nothing new is required, the process is not more difficult or confusing than back in 2020 when we had 1.2 million people regularly renewing coverage.
Wisconsin Unwinding
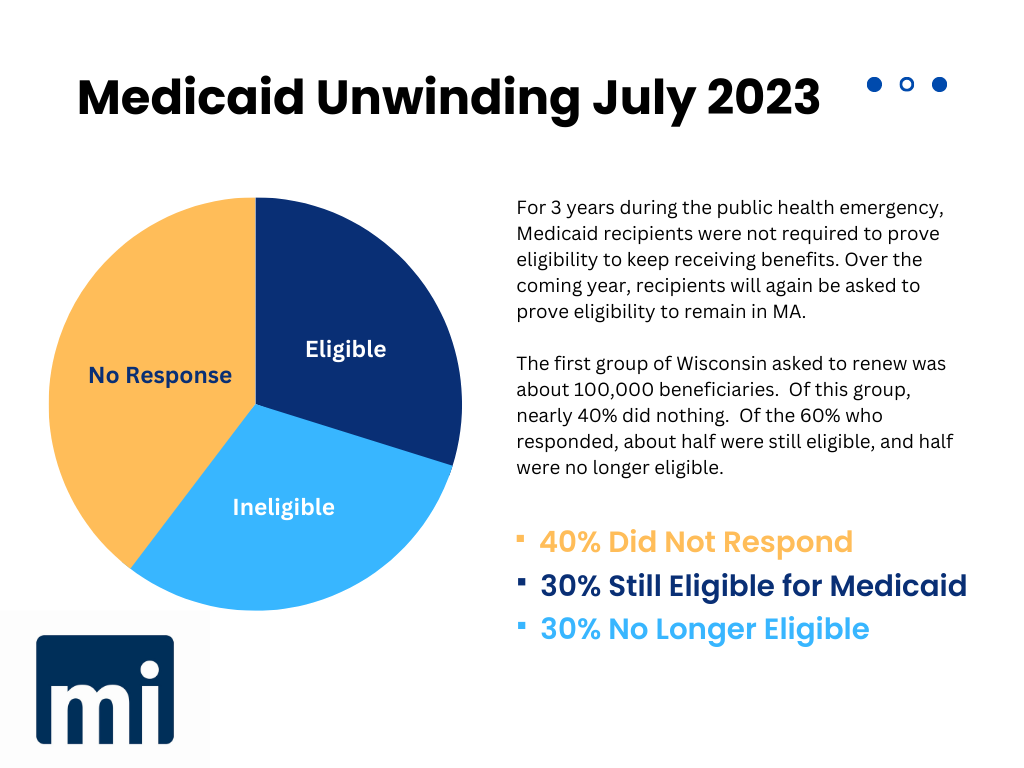
Late last week, the Department of Health Services reported that of the first group of about 100,000 recipients due to renew, close to 40% did nothing to keep their taxpayer-funded health care coverage. Only about half of the recipients who did provide information remained eligible, and according to the department, most of that half no longer met the income criteria for the program.
It’s likely that many of the 40% who didn’t respond to the call to renew know they’re no longer eligible and don’t want to bother. But there appear to be many others, likely still eligible, who didn’t make the small effort required, and will be the first to manage to find a way to complain when they lose coverage.
While recipients will be disenrolled if they fail to renew, there is a three-month period for them to renew without needing to reapply for the program from scratch.
A note about the ‘current address’ issue: Beneficiaries are required to keep their address current, just as they are required to inform the department about changes in income. If Medicaid recipients are abiding by the rules of the program, there should be few wrong addresses. But Medicaid recipients are notoriously non-compliant with keeping their addresses (and likely other information) updated. Again, if states had continued regular eligibility throughout the health emergency (just eligibility checks, even without disenrolling anyone) they could have minimized this concern substantially. And additionally it would have provided valuable information about the number of people who would become ineligible and to get a jump on planning to help transition them to marketplace coverage if needed.
The Biden Administration has halted disenrollment in a dozen states – they refuse to reveal which 12 – because of problems such as states not using electronic data sources to check enrollee’s income so they might be automatically renewed. In other words, some states that are expecting beneficiaries to provide proof of income are being required to stop their unwinding process or risk losing their federal matching dollars if the state doesn’t work to track down income information and auto-renew them.
The Bottom Line
Medicaid is a program that’s meant to cover low-income people in poverty. When states stopped collecting income eligibility information, caseloads ballooned and in Wisconsin alone there are hundreds of thousands of people who are being provided free, taxpayer financed coverage who no longer qualify.
Program integrity requires eligibility checks, and recipients who refuse to provide the basic required information should be disenrolled.
The ‘unwinding’ is nothing more than a return to basic program integrity for the Medicaid program. Recipients should be expected to provide proof of eligibility to continue, on time and without complaining.